A Hyperspectral Sight on the Stain
How advanced imaging technologies are reinventing century-old medical technology
Humans have many characteristics that set us apart from the rest of the animal kingdom: language and speech or the ability to walk upright. But there’s one crucial organ that has left us pretty average: our eyes.
Even with full-color eyesight we can only see within a somewhat narrow spectrum of the electromagnetic scale, wavelengths of about 300 to 400 nanometers. Within that short spectrum, our eyes are sensitive to three colors—red, green and blue. As those colors mix together we see the rest of the colors that we know: the oranges, the yellows, the pinks and purples. As all of those colors can mix into great vibrance, you might think our eyes have the power for some serious viewing—and we do—but only in regular, everyday life.
A pathologist has a very different “everyday,” using their eyes to study and diagnose disease. They do that by probing samples of human tissue through a microscope for clues to help them determine a diagnosis. But pathologists, with our only-average eyesight, can’t rely on their microscope alone for the best results.
Contrast, texture, and color.
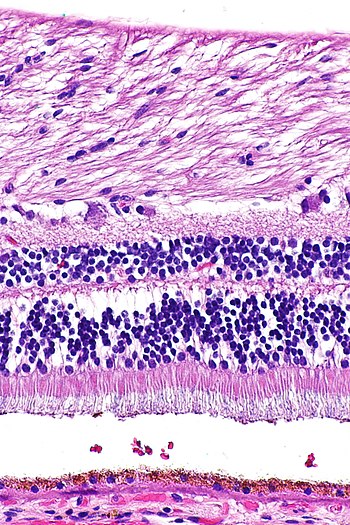
A tissue sample in its natural form is bland and colorless, appearing to be a continuous blob without structure or texture. Even with a high-powered microscope, a tissue sample provides very little insight to its viewer. A standard practice in histology is staining tissue samples to enhance contrast; creating textures and diversity in color, highlighting the shape and structure of cells and even those cells’ components like the nuclei and cytoplasm. Staining samples brings them to life, so to speak, making them more visible to a pathologist.
While there are a variety of medical stains used in histology, the most common stain—the gold standard—is hematoxylin and eosin stain (H&E), which stains samples across a spectrum of indigo and pink, with purples and magentas in between. Think of it like greyscale, or in this case: purplescale.
The contrasts that are exposed in stained tissue allow pathologists to identify and diagnose diseases. But making that identification requires specialized expertise. And with heavier workloads and less-experienced clinicians entering the field to meet demand, the diagnosis process is becoming slower.
A Stain on the System
“97% of departments don’t have enough histopathologists for the workload and that workload is rising,” said Jo Martin, President of the Royal College of Pathologists and Professor of Pathology at Queen Mary University of London. “We know that with every sample, we have to do more with it and that all again adds to the burden.” Pathology departments are struggling to keep up with the workload because new talent isn’t entering the field at the same rate that old talent is leaving. As the pathology population diminishes, pathologists have found the help of computer-assisted automated image analysis systems.
As these image analysis systems begin performing the pathologist’s job, combing the samples, looking for the areas of interest, the AI is running into problems and it has to do with those stains. Although H&E staining has been in practice in medical fields since the late nineteenth century, it comes with its drawbacks—it turns out it’s not so reliable for the new digital methods.
Because histology involves humans, naturally, there are going to be inconsistencies. It often comes down to variability among the individual histologists doing the staining, difference in practice between facilities, the orientation of the specific tissue or specimen, and the overall skill involved in preparing the samples, along with color variation, depending on the variety of stains used in different sample sets.
These variations in staining cause obstacles for the automated image analysis systems that are used to collect data, label samples and digitally catalog collections of tissue samples to be used for digital pathology. With these inconsistencies, similar tissue can appear remarkably different for several reasons, including different chemical formulations, different scanners and lab protocols.
So there’s a question to be asked: if staining samples is causing problems for modern, digital pathology, is there a technology that could highlight characteristics in a sample that stains are missing, allowing pathologists to not have to rely solely on the old practice.
The Center for Machine Vision and Signal Analysis at the University of Oulu in Finland considered this very idea.
A New Look
Scientists are developing a system to virtually stain a medical sample making it possible for unstained specimens to be viewed as if they were stained. With the use of hyperspectral imaging (HSI) technologies, histologists can potentially avoid the costly, lengthy and inconsistent process of chemical staining like H&E, limiting the risk of potentially compromising the sample, and providing pathologists with higher quality samples for precision diagnosis.
HSI, unlike our eyes and other forms of imaging, captures images in a wide spectrum of wavelengths across the electromagnetic spectrum, like ultraviolet and near-infrared. HSI collects data from each pixel in the image and presents it as an information-rich hypercube, where multiple versions of the same image are displayed across many wavelengths. in two spatial dimensions and one spectral dimension.
Image processing techniques, like spectral unmixing, when applied to HSI data provide insights to pathologists that they wouldn’t normally observe by looking at standard microscopy images. Unlike traditional chemically stained samples, the hypercubes collected allow pathologists to view a sample across a wider spectrum of wavelengths. By exposing subtle color and textural differences that are not observable by the naked eye, pathologist are able to identify disease, and when paired with automated imaging systems and machine learning, the ability to recognize and classify similar and different tissue samples takes place autonomously.
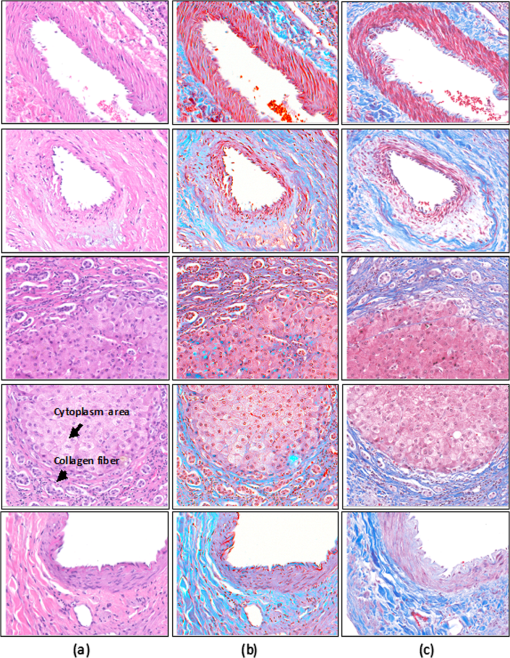
Comparing digitally stained images of fibrous tissue to two chemically stained samples, H&E and Masson’s trichrome—another common staining technique—the difference in detail is quite apparent. In the H&E sample, the difference in color between collagen fiber and smooth muscle is just barely noticeable. In the Masson’s trichrome stained sample, the differences are distinct, as there is more variety in color—more reds and blues as opposed to just pinks and purples. And in the digitally stained samples, the colors are much more vibrant and diverse, resulting in a clearer distinction between collagen fibers and smooth muscle tissue.
What’s next
As HSI rapidly develops and emerges into medical fields like pathology, there are challenges to how data is gathered. Acquiring high-resolution HSI datasets in video rates and extracting that data as high-quality diagnostic information is an example of those challenges. Pathologists will need to establish a digital library of molecular biomarkers, disease-specific endogenous substances and all types of tissue and the ability to process that data fast and autonomously.
Because of the stakes, the field of pathology is necessarily a conservative one. Pathologists are somewhat set in their ways and practice, not very open to the huge changes that HSI brings to how they detect diseases and make their diagnosis. Introducing this arcane technology—so far outside of our everyday experience of the world—into the field won’t happen all at once.



 Conclusion: Mapping the Efficiencies of 3D Digital Pathology
Conclusion: Mapping the Efficiencies of 3D Digital Pathology  Faster, better, stronger: the power of automated 3D histopathology
Faster, better, stronger: the power of automated 3D histopathology 