Under the skin: Diabetes monitoring is using imaging to go new places
Tackling one of the world’s most common diseases with better technologies
Diabetes is one of the most serious and widespread diseases in the world. In some countries, it affects almost a third of the population. It’s expensive to treat. And it’s growing everywhere. In the US alone, the rate of adults diagnosed with diabetes has doubled in the last twenty years.
While exact numbers are difficult to get, they are large. According to the World Health Organization (WHO), there are over 420 million people in the world suffering from diabetes, and another 370 million are at risk of developing type 2 diabetes. The International Diabetes Federation (IDF) reports that about 537 million people worldwide have diabetes. The number of cases has been increasing over the past few decades, and the IDF predicts 783 million people will have diabetes by 2045 — an increase of 46%.
This growth is led by the prevalence of type 2 diabetes, which is rising across all countries. It is likely due to a combination of factors, including economic development and increasing urbanization that often leads to lifestyles with higher risks of developing diabetes, but also an aging global population that is more likely to develop diabetes and live with it for longer.
Diabetes is a chronic disease that affects millions of people around the world. In the United States, 1.5 million people receive a diabetes diagnosis every year.
While there is currently no cure for diabetes, a longer lifespan is an indication of success in medical care: early detection, better self-management solutions, and effective treatment of diabetes have led to longer survival rates that contribute to the rise in prevalence.
Understanding diabetes
A key to improving outcomes has been in improving our understanding of the disease. We’ve known of diabetes mellitus and its symptoms for thousands of years, with descriptions found in Egyptian papyri, ancient Indian and Chinese medical literature, and in the work of ancient Greek and Arab physicians. But it wasn’t until the 19th century that our understanding of the root causes accelerated, leading to the extraction of insulin from the pancreas in 1921 and a new era of medical treatment.
Today we know it as a chronic health condition that hinders the body’s ability to turn food into glucose, the sugar that feeds our cells. We require the hormone insulin to move the glucose from our bloodstream into our cells.
With Type 1 diabetes, the immune system attacks the insulin-producing cells in the pancreas, leaving the body with little or none of the hormone. Its precise cause is unknown, but it is typically diagnosed at a younger age. Type 2 diabetes usually develops later in life, and is more likely caused by lifestyle factors such as diet and exercise, though genetic factors are also significant contributors. A third type of diabetes, Gestational, affects pregnant women and typically lasts until the baby is born. With Gestational and Type 2, the cells in the body become resistant to insulin, and so use it less effectively.
Whether the body doesn’t make enough insulin or can’t use it as well, the result is too much blood sugar staying in the bloodstream. Over time, this can cause a wide variety of serious health problems, including heart disease, vision loss, and kidney disease.
Diagnosing diabetes
Doctors have started screening patients for diabetes. A new term, “prediabetes,” has been coined, which denotes the stage in which blood sugar levels are elevated, but the patient has not progressed to the stage of full-blown diabetes. Doctors recommend only exercises and dietary changes for this category of people. If there is no improvement in blood sugar levels, doctors may consider starting medications.
Because of the easier availability of a new blood test known as HbA1C, it is possible to diagnose diabetes without fasting for 12 hours. The American Diabetes Association recommended the test for routine screening in 2010. The test is a much more reliable test for diagnosing diabetes early. Hence, diabetes is detected much earlier, and young people are getting diagnosed with diabetes.
Managing diabetes at your fingertips
Today a person can live a long and healthy life with diabetes, but that comes with some requirements.
While some Type 2 and Gestational patients can manage their condition through diet and exercise, most living with diabetes rely on different ways of monitoring their condition and then using shots or infusions of insulin to maintain necessary levels. Two important ways of monitoring are levels of glycated hemoglobin, which requires a blood test at a doctor’s office, and blood glucose, which can be done by a patient in their home. The measuring of blood glucose allows the patient to figure out how much insulin they need and when.
This kind of self-management can have significant benefits – reducing blood sugar levels, symptoms, overall mortality risk, and healthcare costs. Staying in your target range can also help improve energy and mood. Missing the target can lead to long-term effects, but there were immediate unpleasant side effects of low blood sugar as well, such as shaking, sweating, nervousness or anxiety, dizziness, and irritability or confusion. These kinds of symptoms can then make it more difficult to get help when it’s needed.
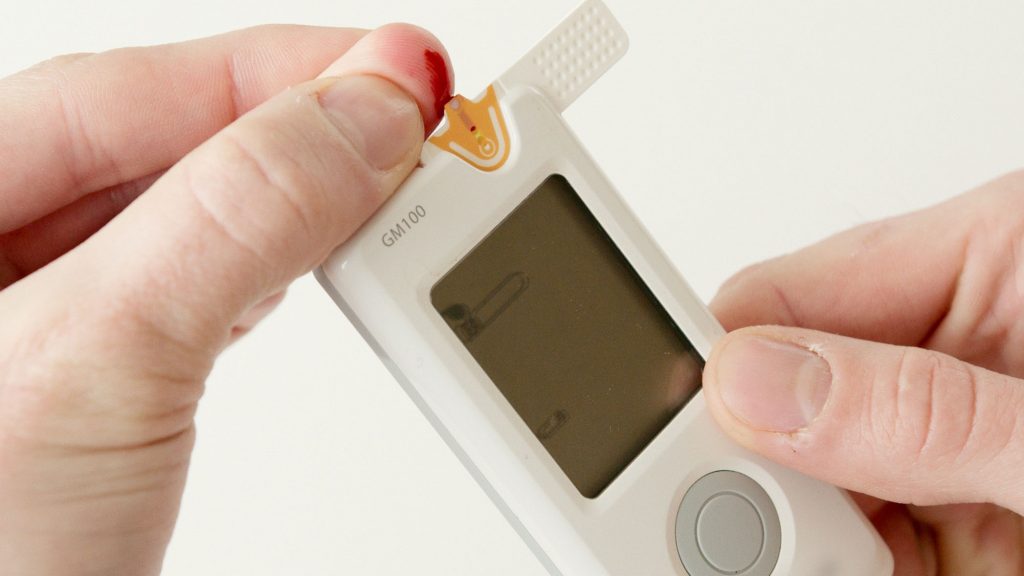
The problem is that it is, quite literally, a pain. In the past, patients typically used a glucometer, which measured the amount of sugar in a small sample of blood, usually by pricking your fingertip. While this enzyme-based method is very accurate, it causes skin irritation to the patients each time, especially when frequent measurements are needed. Test strips are for one-time use only and can become expensive over time. Digital readers can have up-front costs that can keep them out of the market in lower- and middle-income countries.
While the frequency of testing varied by patient and type of diabetes, this meant at least testing several times of day: waking up, before eating or drinking anything, before regular meals, and at bedtime. Measuring too seldom, even 2-3 times a day is not an accurate representation of glucose levels throughout the day. As a result of all factors, patients often discontinue monitoring and treatment or make poorly informed decisions about their own health.
Managing Diabetes with implantable imaging solutions
Clearly an alternative is needed. A newer and increasingly popular approach is a continuous glucose monitor (CGM), which provides real-time information about blood sugar levels. These devices measure at frequent intervals, and a notification system can tell the patient instantly when their glucose levels are too high or too low.
Metabolic diseases require the continuous management of eating habits, diet, physical exercise, and sleep, so consistent data over time from devices like these can be enormously valuable in helping patients and healthcare professionals understand physiological responses to nutrition, physical activity, and patterns in glucose control. The more information that is collected across patients can also lead to bigger opportunities: database-driven algorithms, multimodal information processing, and trend analysis to help inform better predictive alerts and new approaches to managing individual health.
Detecting glucose in the blood, within a living human body, in real-time is not easy – changes in temperature and contact pressure can affect imaging, especially since the reflected glucose signals suffer from strong absorption and weak intensity, affecting accuracy. One approach in an implantable device is NIR imaging sensor assisted by fluorescent dye. The disadvantage of this approach is that the fluorescence is temporary, with commercial solutions lasting only a few months. Electromagnetic sensors that can be implanted beneath the skin and are capable of tracking minute changes in blood glucose by measuring changes around how the blood holds electrical charge have been proposed.
Still, near-infrared imaging seems the most promising, as it can show glucose-dependent intensity variations due to spectral absorption when illuminated, and the reflectance changes with the blood glucose variations.
Today the challenge rests on what kinds of sensors to use in implantable devices to give accurate and reliable measurements. Optical spectroscopic methods have shown some promise: near-infrared (NIR) absorption spectroscopy has been shown to identify glucose-specific features in the presence of many confounding signals. While this imaging approach is non-invasive, it’s not practical for an implantable device.
On top of the sensor challenges, the design of the complete device faces its own complications. If the device is too large, it can be uncomfortable for patients. The materials themselves need to be biologically compatible – solid-state materials like silica can cause infections or prompt immune reactions to the foreign body.
Despite these challenges, many researchers are working on new solutions. A recent feasibility study of a subcutaneous multi-metabolite sensor, funded in part by the EU, indicated that a CGM system could overcome the limitations of existing devices with a solution that is not visible on the patient’s body and requires minimal patient input. The sensor can reliably measure glucose as well as metabolic indicators ketones and lactate. Together, these indicators provide more comprehensive information on fat metabolism and physical activity, helping to predict when glucose levels can be dangerously low or high.
Looking forward
Successful diabetes management can reduce healthcare costs and minimize the associated medical complications for hundreds of millions of people. The costs involved are enormous: the annual global expenditure for healthcare for the disease is more than USD 760 billion and growing. Close to 40% of that is in the United States. Organizations such as the Rand Corporation and the Mayo Clinic have raised the alarm about the high costs of diabetes care and related costs. A combination of new solutions and better technology will be needed to face this growing problem in the future.



