Taking some heat: Thermal imaging for elevated body temperature in 2020
As government and business leaders start to talk about “returning to normal,” and looking to thermal cameras to help, questions remain about “how,” and whether the latest technology can help.
Across industries, we are all looking for the right tools to help detect, slow, and eventually, stop the virus. Beyond that, resuming operations in any way will require demonstrating measures to protect the health and well being of people in a variety of situations, including travel and work.
One proposed solution is thermal scanners. Unlike most medical imaging approaches, IR thermography doesn’t require irradiation or expensive equipment, and presents no health hazard. Infrared radiation emitted from our body can be detected, and with information about the ambient environment, used to to estimate core body temperature and potentially detect who is running a fever. If someone has a higher-than-expected body temperature, they might be running a fever. If they are running a fever, that might mean they are infected with a disease. And if they have a disease causing the fever, it might be Covid-19, as this is a common early symptom.
If this seems a bit indirect, it is. Thermal cameras can’t detect a virus or specific infection. Makers of thermal camera systems and medical experts have had to repeatedly remind people that they can’t be used as such.

But there is a lot that thermal camera systems can do, such as quickly narrow a large pool of individuals to a smaller one. Such systems can come in many forms that include sophisticated fixed-position scanners and basic hand-held thermometers. Increasingly, the most common setups for accuracy for Covid-19 detection are simply cameras attached to a laptop, pointing toward a passageway through which people walk.
At the time of writing, this represents the only viable non-contact mass screening approach for outbreaks of infectious disease pandemics like the recent Ebola disease outbreaks in West Africa, severe acute respiratory syndrome (SARS) outbreak in 2003, and the influenza A pandemic (H1N1) outbreak in 2009. In a busy public environment like an airport, there are simply not a lot of other options. You need nearly real-time estimation of body temperature to identify infectious individuals who require prompt quarantine.
The accuracy of the infrared system can, however, be affected by human, environmental, and equipment variables. Understanding those variables will help both users and system makers deliver the best results. That takes multiple considerations of how the science, technology, and applications themselves interact.
Consideration #1: Think about the user
Thermal detection has been used for fever detection for twenty years. And while camera systems can be more sophisticated, they are not the only option. Particularly in Asia, fast, efficient, and cost-effective IR thermometers have been used in public spaces like airports for screening. A document from the Centers for Disease Control and Prevention provides one reason that thermometers are more accurate than camera-based systems: they may be easier to use effectively.

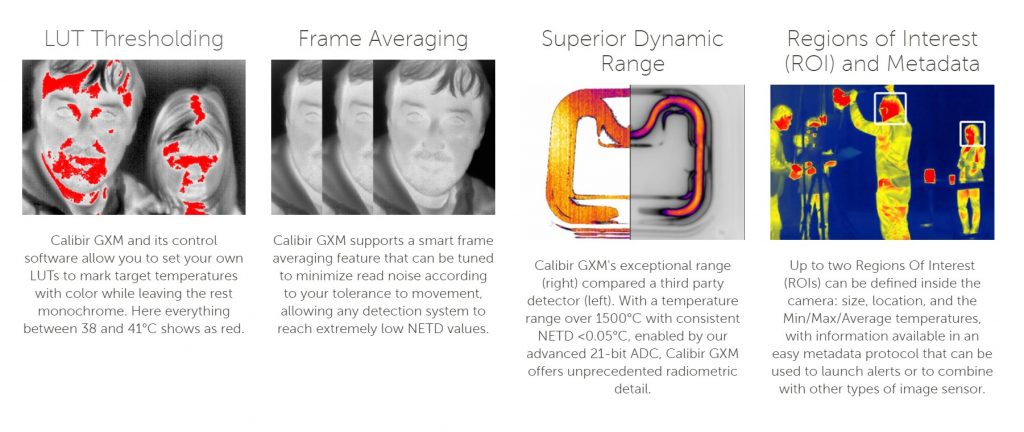
Still, thermometers have their weaknesses. First, they require the user to violate the 6 foot/2-meter social distancing recommendation, increasing risk for everyone. Also, by only measuring temperature in a single spot, they can’t account as easily for variations across surfaces or get a ‘bigger picture’ of body temperature in context (for example, compared to the environmental temperature). In 2015, researchers looking to detect the swine flu had difficulties measuring body temperatures in the hot and humid environment of a Singapore airport. They found that compared to thermometers and older thermal cameras of the type used to detect SARS, the new generation offered significant performance improvements. Some of this had to do with the intelligence of the systems – features like real-time calibration to ambient temperature with sub-degree °C accuracy.
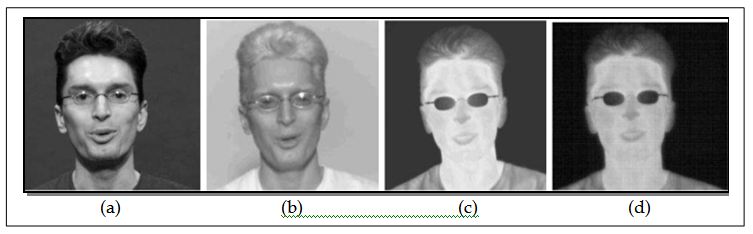
Other key features of the new camera system that led to improved results were user-friendly ones: automated target recognition, improved resolution, pairing of a thermal camera with a visible-light camera, automated alarms for possible febrile cases, and clearer outlining of hot spots. In “Best practices for standardized performance testing of infrared thermographs intended for fever screening,” in 2018, researchers continued to find increasing evidence that cameras are more effective than other methods (including contact thermometers in the mouth or ear).
“There are huge advantages to these kinds of thermal imaging systems,” says Bruno Menard, Software Director at Teledyne DALSA. “Our latest cameras, supported by our imaging tools, can perform initial screenings of people in real-world environments – places like airports and warehouses – where they’re needed.”
One cumulative insight from these findings should help people plan their fever detection approach by considering the system users. Will they have enough training before they start? How much? People can very quickly learn to use IR spot thermometers, but their maximum efficacy is limited. On the other hand, the latest thermal camera systems have enough quality-of-life features to offer significantly more reliable results with only slightly more training.
Consideration #2: Know your baselines
Because the environment can influence temperature measurements, some system makers recommend recording a population baseline at each site on each day: taking about ten known healthy individuals, scan them with the camera and save their readings. Subjects scanned afterwards are then compared to this population baseline. There are several problems with this. Because of the incubation time of viruses, particularly Covid-19, and the unreliability of testing, it’s not always possible to know if someone is “healthy.” There are also significant differences between individuals – there is not yet a standard baseline that we understand. The studies that have cast some doubt on the accuracy of this approach recommend more thorough research that compare the results from test subjects that are confirmed to have fevers.
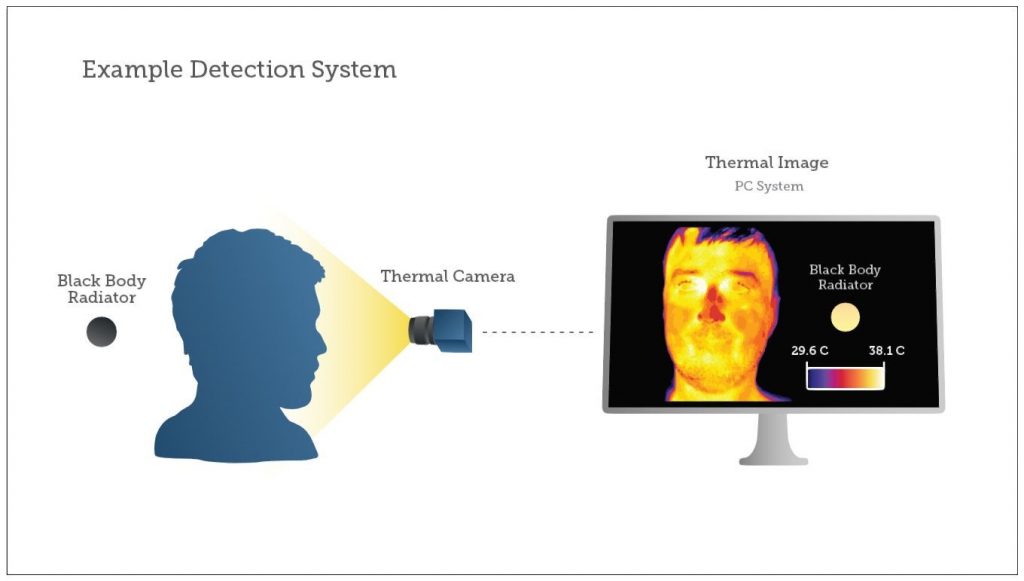
An improved approach is to use a reference temperature source, or “black body.” This is a device designed to maintain itself at a specific temperature or range of temperatures, allowing the thermal camera system to automatically calibrate itself against the temperature it is looking for, even as the ambient temperature changes. The black body needs to be placed in the field of view during the measurement, allowing the imaging software to calibrate the scene to a more precise value than the camera is capable of alone.
Even better is a radiometric camera, which can translate the intensity of an infrared signal reaching the camera into a specific temperature. This requires more rigorous design and testing by the manufacturer, but it delivers much more precise measurements, which as we’ve seen in previous research, delivers better results.
Image uniformity is another critical parameter. In general, the corner areas of the target plane vary much more in lower-quality detectors, making them unreliable and even unusable. A very uniform image across the camera’s field of view means that the camera system has more options in how it is deployed – the subjects don’t have to be in the exact center of the image. Uniformity, along with higher resolution or lower minimum detectable temperature difference, allows for multiple subjects to be accurately measured.
Consideration #3 Looking in the right place
We commonly see thermal imaging system setups that simply point a thermal camera into a crowd. This sort of setup is significantly flawed, when considering all factors that contribute to the accuracy of measuring human elevated body temperature.
While thermal cameras can only detect surface temperatures, different spots on our skin more closely correlate with our core body temperature. If we are using skin temperature as a proxy for what we’re looking for (a fever), we want the best proxy available. More specifically, how skin facial temperature correlates to core body temperature. In the past, the forehead was measured, as it was a large enough target from a distance. Based on more recent scientific research, the most reliable spot in the human face is the canthus, the small corners over the tear duct where the upper and lower eyelids meet.

Several studies suggest that the temperature of the inner canthus of the eye, determined with infrared thermal imaging, is an appropriate method for core temperature estimation in mass screening of fever. The criticism of these studies is most often that measurements were compared to much more error-prone methods, instead of the gold-standard methods of measurements directly from the esophagus or a gastrointestinal telemetry pill. These more accurate tests had much smaller variances when subjects had different levels of activity, such as resting, exercising, and recovering. Some of the realities of modern air travel make all these scenarios possible.
Consideration #4: Checking your distance and performance
While research often carefully examines camera performance one-by-one, out in the field the situation can be more complex. Instead of up-close, people might be (socially) distant. There may be multiple people. People may be wearing makeup, or under physiological stress, sweating, or recently wearing a hat. They may be moving. To give the system a fighting chance, you want to be as close as possible, while balancing issues of safety and efficiency. You also want a camera system with good performance – resolution, sensitivity, and frame rate.
One key constraint of thermal and (long-wave infrared imaging, typically 8-12 µm) is low resolution. While short-wave infrared looks at light reflected from the environment as well as emitted from the subject, thermal imaging looks only at what is emitted from the subject. Less signal means less possible resolution. As a result, thermal cameras tend to work in QVGA and (320 x 240) or more recently VGA (640 x 480), giving systems fewer pixels to work with. Even this is a miracle of modern technology. Not too long ago, industrial thermal imagers were very expensive, $150,000 or more, and very difficult to use, requiring delicate calibration. Today we can talk about them being deployed en masse across airports and stadiums.
Still, the nature of thermal imaging poses a challenge when imaging a subject at a distance. The good news is that we only need about 3 pixels by 3 pixels to get an accurate measurement with the latest cameras. The bad news is our target (the canthus) is tiny, only a few millimeters across.
Greater distances mean fewer pixels on the target. Since the canthus is typically hotter than the surrounding skin, the system may miss the crucial reading. Different lens options will provide the capability to check this small body part according to the distance while still having enough pixels on target to carry out a proper accurate measurement. Indeed different configurations are necessary, depending on how far away the temperature check is being performed, between 0.7 and 10 meters.
“In practice, with a VGA camera, you can properly scan up to four people at a range of 5 meters. There are still a lot of factors to consider, but imaging processing tools are making that easier to manage,” says Arnaud Crastes, business development director in the Uncooled IR division at Teledyne Imaging.

Once again, the black body emitter can help increase the camera’s base accuracy. The black body needs to be placed at an equal distance from the camera as the subject, and a pixel cluster of at least 20×20 pixels covering the emitter will deliver reliable results according to IEC standard. With this approach, the camera can achieve better accuracy taking into account any temperature variation that can happen.
Consideration #5: Finding your way in the “wild west” of thermal imaging in early 2020
In the face of the nuanced considerations of system design and performance, there is a fair degree of chaos. What standards apply to these devices? Which are being enforced? Who makes them? Will they work?
With proper design considerations, thermal camera systems can meet standards such as IEC 80601-2-59 Medical Electrical Equipment: “Particular requirements for the basic safety and essential performance of screening thermographs for human febrile temperature screening,” which included key points such as:
- 320×240 pixel resolution minimum
- Spatial resolution ≤ 1mm (1mrad)
- Accuracy ±0.5°C between 34°C and 39°C
- External 20 x20 pixel black body reference with an accuracy of ±0.3°C and stability < ±0.1°C
- Rainbow colormap and temperature display resolution 0.1°C
As we’ve seen, these kinds of standards are meaningful for the performance of thermal camera systems for fever detection applications. But even if there are standards to meet, it’s not clear whether all companies will be following them, or that they’ll even be enforced. In April 2020, the U.S. Food and Drug Administration warned of a shortage of temperature-reading devices and said it wouldn’t limit pandemic uses of thermal cameras that lack the agency’s regulatory approval.
Hopefully, by deploying this technology as part of a range of measures, businesses and public spaces could potentially begin to reopen without risking a second giant wave of Covid-19 cases. But in preparing for this, organizations are running into another problem: supply. Semiconductor manufacturing in China has been dramatically disrupted in the last few months, and the ripples have been felt across everyone’s technology supply chain.
Even the biggest companies are struggling with supply. Reuters recently reported that Amazon spent nearly $10 million on thermal cameras to check warehouse employees’ temperatures as they reported to work. Since the company is currently using manual thermometers, this would seem to be a big improvement. But the situation became more complicated as the cameras were purchased from Zhejiang Dahua Technology, a company blacklisted by the US government. While sales to private U.S. companies aren’t illegal, it raised yet more security concerns around deploying these systems, particularly when integrated with other systems, such as facial recognition and keycard access to secure sites.
Amazon claims it’s hardware complied with national, state and local law (though that might not be enforced, currently) and says its temperature checks are designed to “support the health and safety of our employees, who continue to provide a critical service in our communities.” And that’s surely what every company wants. For the many industries that have been devastated by this pandemic – including travel, sports, manufacturing, food and hospitality, people are looking for ways to open while keeping people safe and preventing the further spread of the coronavirus.
“For our whole industry, solutions to this unprecedented challenge will require both technology leadership and diligent attention to customer needs,” says Edwin Roks, Group President of Teledyne Digital Imaging. “We are fortunate to be able to combine our advanced semiconductor fabrication with our proven imaging solutions to address this global pandemic. There aren’t easy answers, so close collaboration and evaluation will be our approach every step of the way.”



 Genomics takes its place in the race against COVID-19
Genomics takes its place in the race against COVID-19  Outsmarting global killers: COVID-19 fuels new research on artificial intelligence in healthcare
Outsmarting global killers: COVID-19 fuels new research on artificial intelligence in healthcare 