These Lovely Megapixels Might Save Our Lives
Why making pathology–the up-close diagnosis of our tissues–digital can lead to faster, better treatment.
Anyone who has researched medical symptoms online comes away slightly terrified. You can instantly find dozens of contradictory sources offering very confident diagnoses of your symptoms as something terrible. Blurry vision? It might be diabetes, cancer, rickets, or myopia. Or all of them.
Even if your diagnosis isn’t at all correct (It’s not—you just have dry eyes today), the research and diagnosis process gives you a sense of why it’s a difficult task. The availability of lots of information, wide variation between patients, the difficulty of getting time-consuming medical tests, and potentially high stakes all contribute to making medical diagnosis a difficult thing to do.
Medical experts struggle with this every day. “There is probably nothing more cognitively complicated” than a diagnosis, says internist Mark L. Graber, founding president of the Society to Improve Diagnosis in Medicine “and the fact that we get it right as often as we do is amazing.” He is a leading researcher in the field of medical errors.
A Global Challenge
The stakes are indeed high. Diagnoses that are missed, incorrect or delayed are believed to affect 10 to 20 percent of cases, far exceeding drug errors and surgery on the wrong patient or body part, both of which have received considerably more attention in the news. In another study, pathologists correctly diagnose abnormal, precancerous cells only about half the time, says Dr. Joann Elmore, a University of Washington researcher.
The reasons for this do not usually have to do with the physician’s competency or commitment, but instead how human beings work. Some misdiagnoses are due to overconfidence or a less-than-open mind. We are much more likely to agree with someone else’s opinion. We are also bad at looking through repetitive, barely differentiated imagery for subtle differences in a diagnostic slide that might reveal something like cancer.
The pace of change and the rate of adoption both matter. As the majority of the Western world faces an aging population, looking for a better diagnosis can have both societal and financial implications at a national scale. Earlier diagnosis means that diseases like cancer can be treated earlier, leading to better outcomes. Not only can medical treatment be more efficient, it can be more successful!
In every country, misdiagnoses have been made in the thousands, where invasive procedures might never have happened. Even if the diagnosis is correct (which it most often is), storing physical samples can lead to mistakes, where mislabeled slides or even misplaced ones can be the culprit.
These are hard tasks for humans. But managing this kind of scale and complexity of information is exactly the kind of task that computers excel at.
Enter the New Pathology
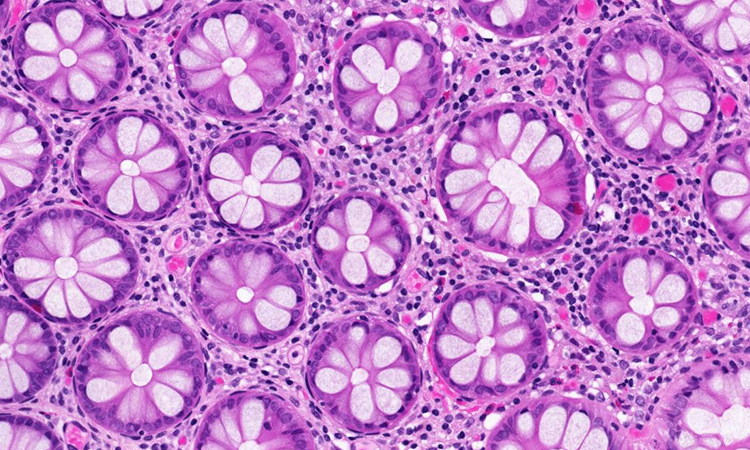
So now new technology is making headway into the front lines of this problem: pathology. Similar to the transformation that radiology departments have experienced over the last decade, new technologies are being introduced, workflows disrupted, and assumptions questioned. Pathology involves analyzing clinical abnormalities that are known markers or precursors for diseases. The lingua franca of pathology is the slide—that sandwich of glass carrying tissue, cells, and body fluid samples.
Pathology as it largely exists today is performed by humans squinting down the moving barrel of a microscope. They slowly change the depths of field to chase cells around a slide. It is difficult work: a highly trained expert pathologist can only work about six productive hours a day. This is to protect their eyesight, and likely their sanity, as these are extraordinarily subtle clues they are looking for. Because the workflow is so dependent on individual interpretation, there are scant quality controls in place and reports that suggest few pathologists would agree with their first assessment when shown the same slide later. The detection and classification of abnormal cells is a subjective exercise reliant on human vision for potentially life and death decisions.
There is probably nothing more cognitively complicated than a diagnosis.
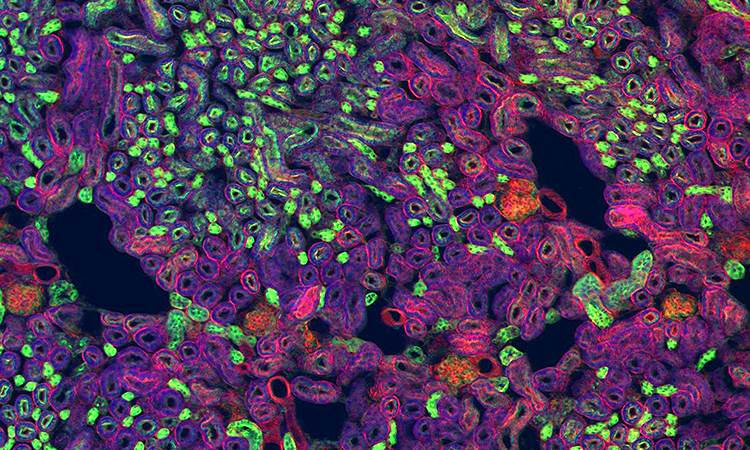
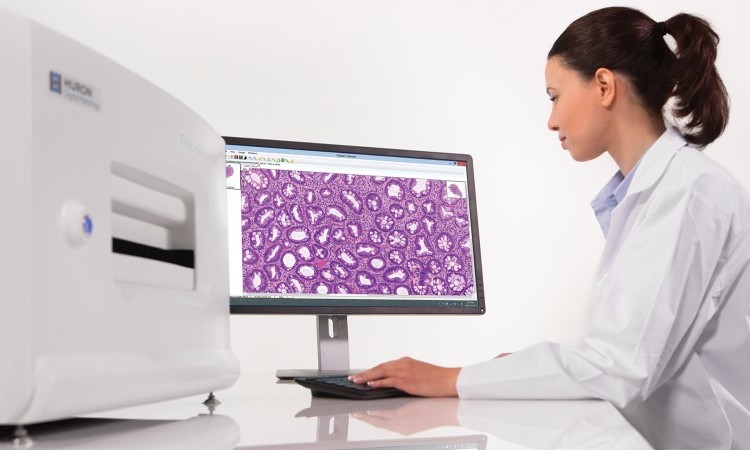
Digital image-based information systems enable the capture, analysis and storage of very high-resolution medical information generated from a digital capture of a slide sample. The field has grown quickly in the last few years, and is one of the most promising avenues of diagnostic medicine that could immediately enable more accurate and timely health care. Integration of reports into the clinical record, digital referrals, harmonization of standards and use of population level data all contribute to safer and better patient care.
This also presents challenges in the context of resource constraints and different commissioning models. The prospect of wider patient access to pathology records is stimulating and challenging to both the professionals and in the development of infrastructure.

“Have a look at what I just sent you”
The future holds some exciting possibilities for collaboration and sharing among a broader range of disciplines and organizations. With portability, comes improved diagnosis – the ability to share digital files to remote experts. By sharing the diagnostic slides as data, new opportunities open up.
Today, it is very difficult (or impossible) to review older archived analog slides. With a digital file, developments can be marked, stored, and referenced later when new slides are taken. One pathologist can make determinations, and then have that work checked by a second pathologist. This could also allow multiple different specialists from around the world to collaboratively triage solutions for difficult cases. One study looked at the challenges of sharing diagnostic information among 20 different healthcare facilities across 100 diagnostic anatomic pathologists.
Let the Machine Do It
Analysis is another important advantage of digital diagnostic slides. Instead of requiring a pathologist to look at everything on every single slide, computer-aided diagnostic tools can find areas of interest faster while improving the accuracy and reproducibility of pathologists’ interpretations. By eliminating inter/intra-observer variability, clinicians get more standardized and reliable information back from the lab. This standardization will also support research efforts that need larger, more consistent data sets.
Whole Slide Imaging
There are a lot of ways to try to capture the deep and crucial information contained in just one slide. Slide samples range in thickness, depending on the tissue and what the pathologist is looking for. Any digital solution has to provide an adequate depth of information from the slide so that the digital copy can be referred to confidently. While medical microscopes can magnify subjects up to 1000x, digital pathology systems tend to go up to 40x, which is sufficient for most diagnoses. Unlike glass slides, which can be lost, fade or damaged with time, images can be archived and retrieved easily.
Approaches to imaging a diagnostic slide range from single plane scan to more complex digital imaging with three-dimensional images in multiple planes (z-stacking). In both approaches to whole slide imaging (WSI), one digitally captures the entire stained tissue specimen on a glass slide. Depending on the system used, various magnifications, scanning methodologies, hardware, and software are employed to convert the optical image of the slide into a digital whole slide image. Specialized viewing software, a “virtual microscope,” makes it possible to get multiple kinds of views of the slide, and have annotations and clinical metadata presented with the image.
What Will the Future Hold?
The adoption rate for digital pathology has been slow, accelerating only recently. Many pathologists have been reluctant to disrupt their existing laboratory workflows. The counter-argument from younger pathologists has been essentially “How do you break something that is already broken?” Many laboratories use manual, fragmented, and inefficient workflows that are very vulnerable to even administrative errors. Digital pathology has made these workflow inefficiencies more apparent.
Adoption of digital pathology needs to accelerate soon. Projections in the United States show a decreasing population of pathologists as more retire and fewer choose the profession. Beginning in 2015, the numbers of pathologists retiring will increase precipitously, a decline that is anticipated to peak by 2021. These fewer pathologists will need to do much more.
Technology is clearly the answer. While human vision will continue to play a crucial role in pathology, digital solutions will allow for more diagnoses that are more accurate, as the review of slides for key information will be easier, and individual pathologists can better leverage the expertise of others. That’s a future worth working towards!



 The Solid State Revolution: Digital X-ray Imaging Goes 3D
The Solid State Revolution: Digital X-ray Imaging Goes 3D  Seeing the Unseen with Microbolometer Technology
Seeing the Unseen with Microbolometer Technology 