AI and medical imaging: building a relationship on solid data foundations
The reasons and concerns behind augmenting traditional medical diagnosis using machine learning
Have you ever seen a Computerized Tomography (CT) scanner? If you ever get the chance to look at one closely, you might feel impressed: it’s a feat of meticulous engineering, capable of simultaneously taking X-rays from hundreds of different angles. You might also feel grateful – it’s one of the most important medical diagnostic advances of the last several decades (with a Nobel Prize behind it).

The powerful processor inside the CT scanner reconstructs a three-dimensional representation, using image processing techniques that carefully examine the image and identify areas of interest. Medical imaging is perhaps today the most advanced and widely practiced branch of medical diagnosis. It surely is hard to believe that this field emerged from an accidental discovery.
In 1865, Röntgen was surprised when he observed that a cathode-ray tube caused different items in his lab to glow. He then experimented with it and realized that this ray could pass through human tissue, but not bones. He called his discovery an “X” ray to communicate his inability to explain the nature of this kind of radiation. A long time passed before ultrasound sensing, originating in maritime warfare technology, was used to search for tumors in the 60s. Magnetic Resonance Imaging, first discovered in the 70s, uses strong magnetic fields and works based on the property that tissues emit different signals depending on their composition, and is now widely used today to detect cancerous cells.
Since then, progress in the field of medical imaging has moved from discovering new techniques of portraying the human body to perfecting existing ones. Computers were introduced and equipped CT scanners in 1972, making it possible to apply image analysis techniques on the generated images. Reduction in cost, harmful side-effects to patients and inaccuracies were of paramount importance to make these practices beneficial and safe for the public. The software employed by medical imaging systems, the operating systems and the image analysis techniques, have become the focal point of progress.
Today, medical imaging is entering a new era, focusing on unlocking the true power of the images themselves. These images, produced by medical systems, vary significantly across applications, but can all be viewed as data useful for medical diagnosis. This new turn is not a coincidence. Our society is currently leveraging the power of data in many other commercial and scientific sectors, from marketing to autonomous driving and climate change. The technology that served as a catalyst in all these cases is Artificial Intelligence (AI), and, when it comes to healthcare, this transition from traditional to AI-enabled practices merits a closer look.

Today, AI researchers are collaborating with physicians to improve medical diagnosis and, in the past couple of years, we have seen systems that successfully use AI for the detection of eye disease, cancer and Alzheimer’s. While slow, AI is steadily penetrating the traditional field of healthcare, as reported in the AI Index 2018 report.
But why has artificial intelligence found such fertile ground in healthcare?
Targeting efficiency and consistency in medical diagnosis
Developing advanced medical imaging created a new problem: we were generating health data quicker than we were able to process it using traditional methods. Roughly 90 per cent of all data comes from imaging technology. It is estimated that at any given time in the UK, there are more than 300,000 X-rays that have been waiting more than 30 days for analysis.
Medical data are only useful when they contribute to medical diagnosis. According to a study, pathologists correctly diagnose abnormal, precancerous cells only about half the time. Also, pathologists are restricted by their human nature: more than six hours of work can be strenuous for them, while a human mind cannot simultaneously analyse more than a handful of pictures to reach a verdict.
AI has long established its success in discovering patterns across vast data sets and reaching conclusions as to the nature of data. Machine learning algorithms observe large data sets of images, discover patterns associated with the presence or absence of a particular disease, and learn prediction models that can be used for medical diagnosis. Deciding whether a tumor is malignant or benign can be viewed as a classification task and data offered from past diagnosis of human practitioners are fed into prediction models to discover what makes a correct diagnosis.
Although immense effort and care are put into the training process, once a model has been correctly validated, it can be a consistent and tireless physician that we can consult whenever we need a diagnosis in the future.
Should we then expect AI to replace the less efficient and more prone-to-error human physicians?

Understanding the limitations of artificial intelligence
Trustworthy prediction models are of immense use, but medical diagnosis is an intricate process consisting of many steps. It follows then, that for one of the steps to fail, could lead to a wrong, and perhaps dangerous, diagnosis.
The most straightforward restriction in AI is its need for data generated by humans. There are a lot of hurdles in this step. Generation requires human resources, time and money, acquisition of data is restricted by privacy laws and, even after data have been collected, the lack of a common interface across different imaging systems, practitioners and countries, leads to the creation of enormous, unstructured databases. These databases are scary enough to discourage any machine learning team from pre-processing them, meaning that a surprisingly large amount of these data does not contribute to medical diagnosis in the end.
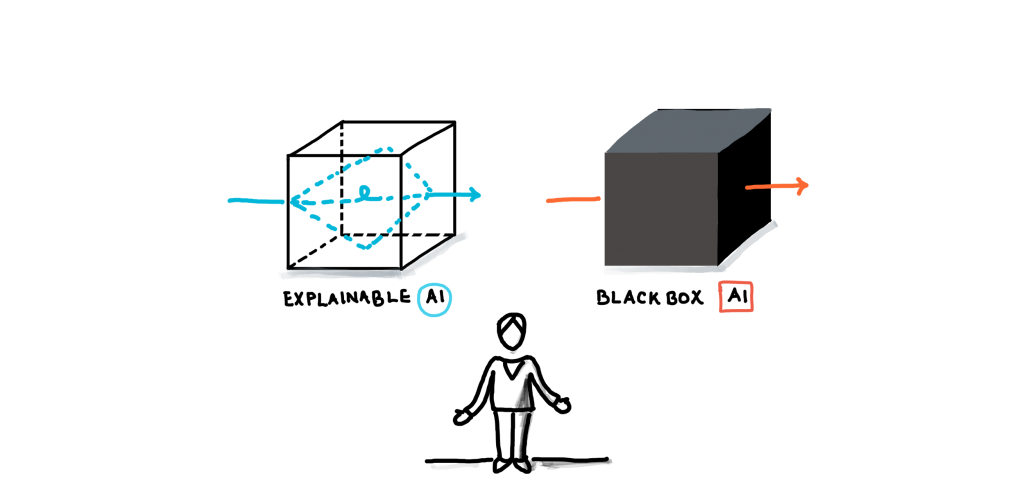
Another important fact about AI that any human physician should bear in mind when interacting with it, is that a prediction model is not a black box offering prophecies that should be blindly trusted. Models are of a purely statistical nature and their decisions should be tuned in accordance with a physician’s understanding of a disease: should the model be conservative when predicting the presence of a disease, or alarm at the slightest chance of a bad diagnosis? Has the model “seen” enough patients in the past similar to the one currently under examination? The human operator should leverage all of their available context to evaluate, and even question, the decisions of the AI system.
This is a great challenge today and has sparked controversy among AI experts, with one side claiming that complexity and deepness of a machine learning model consistently performs better than human intuition and experts on the other side warning that future progress in the field requires explainable AI. When it comes to applications such as healthcare, researchers, practitioners and institutions tend to agree that AI should be viewed as a tool – and how useful can a tool that you can’t understand be?
Finally, when AI is used in a way that directly affects human life, ethical concerns naturally arise. As with autonomous vehicles, medical diagnosis raises the question of liability: who is responsible if a mistake made by an AI system threatens a human life? As diagnosis is a complex procedure that requires the collaboration of different components, our society needs to develop an understanding and a legal framework for addressing these ethical concerns.
A focus on augmentation
Our society is still today pestered by inefficient and unreliable processes, but one should not be carried away by our contemporary urge for automation. Medical diagnosis is an intricate area that differs from other AI applications, such as industrial processes and virtual assistants, in that complete automation is not desired. We will always need human physicians for decision making, interacting with patients and advancing this field with new technologies and ideas.
The essence of augmentation lies in the complementarity of artificial and human intelligence: the advanced analytical skills of AI can be combined with the human abilities of creativity and intuition to bring us one step closer to our quest for efficient, human-centric medical diagnosis. Already, machine learning models are used in AI-based predictive patient surveillance systems, such as WAVE, where they can leverage in real-time data provided by wearables, while SubtlePET and SubtleMR are the first AI-enabled solutions that recently received FDS approval. Although they do not provide medical diagnosis, these systems seamlessly improve the efficiency of existing PET and MRI scanners by enhancing the image quality, accelerating scanning and reducing radiation levels through the use of advanced deep learning algorithms.
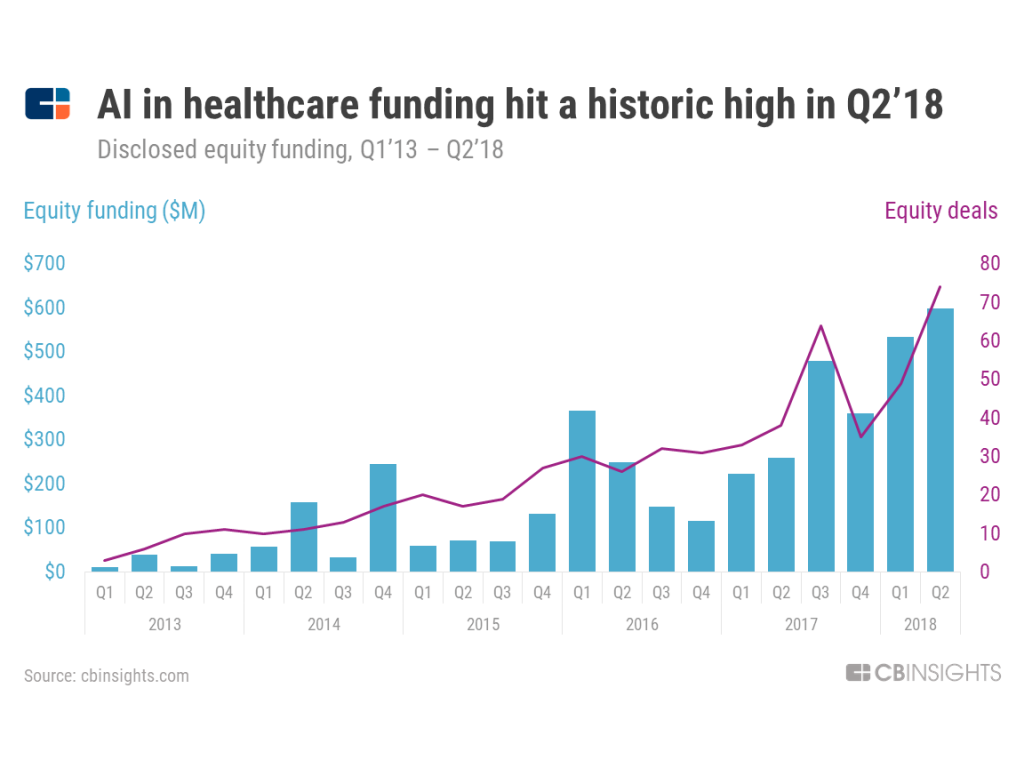
If anything, innovation will continue to accelerate. Within the last five years, healthcare AI startups around the globe raised over $4.3 billion across 576 deals, beating every other industry in terms of deal activity related to artificial intelligence. While this is exciting, there’s plenty of call for caution.: as with all relationships, this collaboration of artificial and human intelligence needs some time to mature and find a balance that augments the strengths and counteracts the weaknesses of the two parts.



